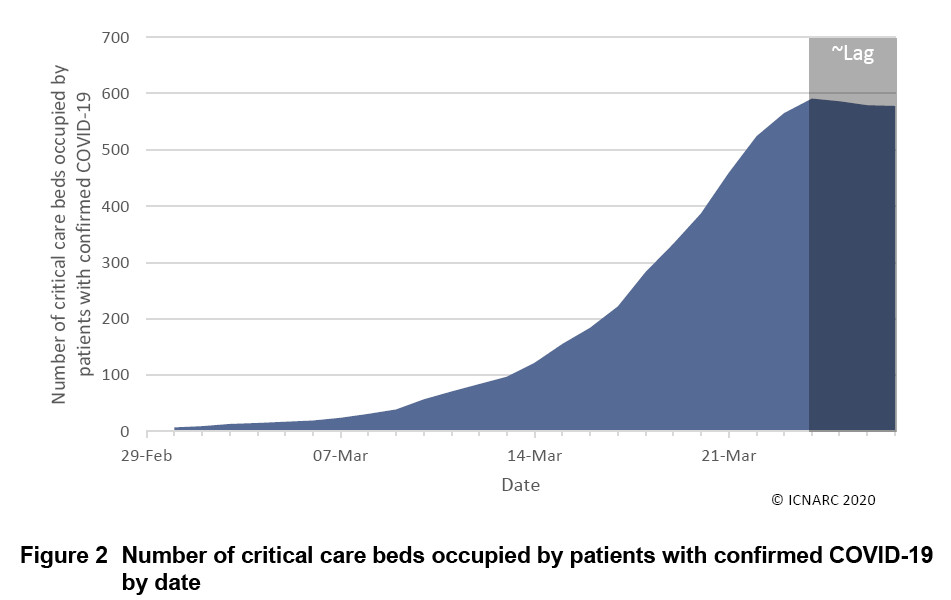
ICNARC’s new “Covid-19” report: the disease is still discriminatory (despite efforts to find young and healthy victims); peak hinted at?
The Intensive Care National Audit and Research Centre (ICNARC) has released another report regarding so-called Covid-19 patients admitted into critical care units, and as reported to ICNARC up to midnight on 26 March 2020. A previous one of these was the subject of a recent FBEL article. The latest ICNARC report presents data of 775 patients, of whom 79 have died, and 86 have been discharged alive from critical care, with 609 being last reported as yet remaining in critical care (one patient appears to have become unaccounted for).
In an interesting development, this new report compares data for Covid-19 patients with that pertaining to 5755 viral pneumonia cases, between 2017 and 2019, of patients who were critically ill in that respect. Presumably, these are also patients admitted to critical care units.
The problem with the exercise in comparing the two sets of data is that the one for Covid-19 is too small. If 75% of 88 women like a hair product, it isn’t by any means a ringing endorsement. The ICNARC report states that of the 165 patients whose outcomes in critical care units is known, 79, or 47.9% have died. Undoubtedly, this high percentage rate will not survive when the other 610(?) patients achieve a known outcome, and here is a piece of evidence for the statement: in the previous ICNARC report, 16 of 33 patients died: 48.5%. As the sample group has grown, the percentage of those who died has shrunk. The set containing the number of viral pneumonia cases is 7 times larger than the one with Covid-19 – when there is equality with this figure (according to a graph, with the two points of ICNARC data plotted on it, and with a line extended exponentially), the percentage for Covid-19 death is dipping below 30%. And this percentage starts to look more like the one given for viral pneumonia deaths in the ICNARC report: 22%.
There is another problem in that comparing Covid-19 and viral pneumonia is like trying to measure something against a ghost. The death that Covid-19 reporting is covering up (which is the subject of the most recent FBEL article) could be a range of things from the severe comorbidities that the ICNARC report lists, to other health conditions that will not register as such but effect the likelihood to die, for instance: old age, previous medication, current treatment, and of course hidden flu and other viral illness. We might call these “hidden” contributory conditions. In other words, the Covid-19 data set is erroneously exaggerated, and it was already too small (and as such, the real percentage for Covid-19 deaths discussed above will be even closer to, if not lower than the one for viral pneumonia deaths).
The most useful figures in the ICNARC report are the ones that contrast the qualities of the “Covid-19” patients who are discharged from critical care against the qualities of the “Covid-19” patients who die in critical care. Using the pronoun “he” (because there is some variation between men and women patients) for general discussion, these figures tell us the following:
A Covid-19 patient is more likely to die the older he is, and less likely the younger.
A Covid-19 patient is more likely to live when his Body Mass Index is less than 30, but when it is more than 30 (denoting obesity), the patient is more likely to die. Naturally, one must then want to know if these patients would have been identified by the NHS for obesity medication, or even been subjected to medicine for other related illnesses (see this FBEL article for the relevance).
A Covid-19 patient is more likely to die if he requires daily assistance with living, and more likely to survive if he does not: perhaps suggesting that there is a hidden condition related to old age (or decrepitude) to be considered in patients that do die.
A Covid-19 patient is more likely to die if he has a severe comorbidity, and more likely to survive if he does not. This is self-explanatory.
A Coviod-19 patient is more likely to die if he has received advanced respiratory support, and more likely to survive if he has not. The question as to whether the treatment cures or fails in all cases, or if it in fact sometimes kills, could apply here.
To summarise, there is not a concept about Covid-19 that has thus far been established (i.e. that it hurts the weakened) that is not contradicted by the ICNARC report.
The most fascinating part of the report, however, is the graph (above) that shows the number of critical care beds occupied by patients with confirmed Covid-19 dipping in the period spanning from the 23rd to the 27th March. The ICNARC provides a caveat for this graphic: it is “affected by a variable lag time in submission of data of about 1-3 days (shaded grey)”. It means that the shape of the graph will probably, and surely change (upwards). That being said, in its current shape it is an indicator that occupancy of critical care beds is not being sustained by rates of new patients. We will wait to see how this develops, bearing in mind that Imperial College statisticians have now envisioned 5,700 deaths (in total?) with Covid-19, and that a date for the arrival of the peaking of the disease has now solidified (in what was a previously liquid narrative) as being the Easter weekend. And about this particular piece of data, although Dr Jenny Harries, the Deputy Chief Medical Officer for England, may have given an impression, at the daily Covid-19 incident briefing yesterday, that this peak was due to the UK Government’s lockdown, it is in fact a premature event according to the Imperial College’s model for the impact of full mitigation measures, and a forced adaptation based on lower estimates for death – as reported here at FBEL.